| Knee Replacement
What is Knee Replacement?
 Your
knees work hard during your daily routine, and arthritis
of the knee or a knee injury can make it hard for
you to perform normal tasks. If your injury or arthritis
is severe, you may begin to experience pain when you
are sitting down or trying to sleep. Your
knees work hard during your daily routine, and arthritis
of the knee or a knee injury can make it hard for
you to perform normal tasks. If your injury or arthritis
is severe, you may begin to experience pain when you
are sitting down or trying to sleep.
Sometimes a total knee replacement
is the only option for reducing pain and restoring
a normal activity level.
If your and your doctor decide a
total knee replacement is right for you, the following
information will give you an understanding about what
to expect.
A total knee replacement involves
replacing the damaged bone and cartilage of the knee
joint, which provides articulating surfaces.
The total procedure takes approximately
an hour to hour and a half to perform and recovery
time varies between patients. Correct rehabilitation
following surgery significantly improves outcomes.
Implant Components
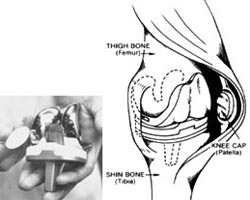
In the total knee replacement procedure,
each prosthesis is made up of four parts. The tibial
component has two elements and replaces the top of
the shin bone (tibia). This prosthesis is made up
of a metal tray attached directly to the bone and
a plastic spacer that provides the bearing surface.
The femoral component replaces the
bottom of the thigh bone (femur). This component also
replaces the groove where the patella (kneecap) sits.
The patellar component replaces
the surface of the kneecap, which rubs against the
femur. The kneecap protects the joint, and the resurfaced
patellar button slides smoothly on the front of the
joint. This may or may not be replaced depending on
the condition of the patient.
Advantages of Total Knee Replacement
The most important advantage is
that this operation produces very effective and long
lasting relief from joint pain. It also gives a joint
which functions normally. The recovery period from
the operation is very short and the patient is able
to walk from the second or vthe third day after the
operation. Walking support that is needed can often
be discarded by around a month's time. The patient
regain a normal lifestyle and mobility with significant
improvement in quality of life.
Exercise Program and Physical Therapy/
Rehabilitation after Knee Surgery
Knee replacement surgery is a complex
procedure, and physical knee rehabilitation is crucial
to a full recovery. In order for you to meet the goals
of total knee surgery, you must take ownership of
the rehabilitation process and work diligently on
your own, as well as with your physical therapist,
to achieve optimal clinical and functional results.
The knee rehabilitation process following total knee
replacement surgery can be quite painful at times.

Your knee rehabilitation program
begins in the hospital after surgery. Early goals
of knee rehabilitation in the hospital are to reduce
knee stiffness, maximize post-operative range of motion,
and get you ready for discharge.
When muscles are not used, they
become weak and do not perform well in supporting
and moving the body.
Your leg muscles are probably weak
because you haven't used them much due to your knee
problems. The surgery can correct the knee problem,
but the muscles will remain weak and will only be
strengthened through regular exercise. You will be
assisted and advised how to do this, but the responsibility
for exercising is yours.
Your overall progress, amount of
pain, and condition of the incision will determine
when you will start going to physical therapy.You
will work with physical therapy until you meet the
following goals:
1. Independent in getting in and
out of bed.
2. Independent in walking with crutches or walker
on a level surface.
3. Independent in walking up and down 3 stairs.
4. Independent in your home exercise program.
Your doctor and therapist may modify
these goals somewhat to fit your particular condition.
In your physical therapy sessions
you will walk, using crutches or a walker, bearing
as much weight as indicated by your doctor or physical
therapist. You will also work on an exercise program
designed to strengthen your leg and increase the motion
of your knee.
Your exercise program will include
the following exercises:
Quadriceps Setting
The quadriceps is a set of four
muscles located on the front of the thigh and is important
in stabilizing and moving your knee. These muscles
must be strong if you are to walk after surgery. A
"quad set" is one of the simplest exercises
that will help strengthen them.
Lie on your back with legs straight,
together, and flat on the bed, arms by your side.
Perform this exercise one leg at a time. Tighten the
muscles on the top of one of your thighs. At the same
time, push the back of your knee downward into the
bed. The result should be straightening of your leg.
Hold for 5 seconds, relax 5 seconds; repeat 10 times
for each leg.
You may start doing this exercise
with both legs the day after surgery before you go
to physical therapy. The amount of pain will determine
how many you can do, but you should strive to do several
every hour. The more you can do, the faster your progress
will be. Your nurses can assist you to get started.
The following diagram can be used for review.
Terminal Knee Extension
This exercise helps strengthen the
quadriceps muscle. It is done by straightening your
knee joint.
Lie on your back with a blanket
roll under your involved knee so that the knee bends
about 30-40 degrees. Tighten your quadriceps and straighten
your knee by lifting your heel off the bed. Hold 5
seconds, then slowly your heel to the bed. You may
repeat 10-20 times.
Knee Flexion
Each day you will bend your knee.
The physical therapist will help you find the best
method to increase the bending (flexion) of your knee.
Every day you should be able to flex it a little further.
Your therapist will measure the amount of bending
and send a daily report to your doctor.
In addition, your therapist may
add other exercises as he or she deems necessary for
your rehabilitation.
Straight Leg Raising
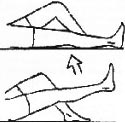 This
exercise helps strengthen the quadriceps muscle also.
Bend the uninvolved leg by raising the knee and keeping
the foot flat on the bed. Keeping your involved leg
straight, raise the straight leg about 6 to 10 inches.
Hold for 5 seconds. Lower the leg slowly to the bed
and repeat 10-20 times. This
exercise helps strengthen the quadriceps muscle also.
Bend the uninvolved leg by raising the knee and keeping
the foot flat on the bed. Keeping your involved leg
straight, raise the straight leg about 6 to 10 inches.
Hold for 5 seconds. Lower the leg slowly to the bed
and repeat 10-20 times.
Once you can do 20 repetitions without
any problems, you can add resistance (ie. sand bags)
at the ankle to further strengthen the muscles. The
amount of weight is increased in one pound increments.
Use of heat and ice
Ice : Ice may be
used during your hospital stay and at home to help
reduce the pain and swelling in your knee. Pain and
swelling will slow your progress with your exercises.
A bag of crushed ice may be placed in a towel over
your knee for 15-20 minutes. Your sensation may be
decreased after surgery, so use extra care.
Heat : If your
knee is not swollen, hot or painful, you may use heat
before exercising to assist with gaining range of
motion. A moist heating pad or warm damp towels may
be used for 15-20 minutes. Your sensation may be decreased
after surgery so use extra care.
Long-Term Knee Rehabilitation Goals
Once you have completed your knee
rehabilitation therapy, you can expect a range of
motion from 100-120 degrees of knee flexion, mild
or no pain with walking or other functional activities,
and independence with all activities of daily living.
Guidelines at Home - What happens
after I go home?
Medication
- You will continue to take medications as prescribed
by your doctor.
- You will be sent home on prescribed medications
to prevent blood clots. Your doctor will determine
whether you will take a pill (Warfarin or coated
aspirin) or give yourself an injection. If an injection
is necessary, your doctor will discuss it with you,
and the nursing staff will teach you or a family
member what is necessary to receive this medication.
- You will be sent home on prescribed medications
to control pain. Plan to take your pain medication
30 minutes before exercises. Preventing pain is
easier than chasing pain. If pain control continues
to be a problem, call your doctor.
Activity
- Continue to walk with crutches/walker.
- Bear weight and walk on the leg as much as is
comfortable.
- Walking is one of the better kinds of physical
therapy and for muscle strengthening.
- However, walking does not replace the exercise
program which you are taught in the hospital. The
success of the operation depends to a great extent
on how well you do the exercises and strengthen
weakened muscles.
- If excess muscle aching occurs, you should cut
back on your exercises.
Other Considerations
- For the next 4-6 weeks avoid sexual intercourse.
Sexual activity can usually be resumed after your
6-week follow-up appointment.
- You can usually return to work within two to
three months, or as instructed by your doctor.
- You should not drive a car until after the 6-week
follow-up appointment.
- Continue to wear elastic stockings (TEDS) until
your return appointment.
- No shower or tub bath until after staples are
removed.
- When using heat or ice, remember not to get your
incision wet before your staples are removed.
Your Incision
Keep the incision clean and dry.
Also, upon returning home, be alert for certain warning
signs. If any swelling, increased pain, drainage from
the incision site, redness around the incision, or
fever is noticed, report this immediately to the doctor.
Generally, the staples are removed in three weeks.
Prevention of Infection
If at any time (even years after
the surgery) an infection develops such as strep throat
or pneumonia, notify your physician. Antibiotics should
be administered promptly to prevent the occasional
complication of distant infection localizing in the
knee area. This also applies if any teeth are pulled
or dental work is performed. Inform the general physician
or dentist that you have had a joint replacement.
You will be given a medical alert card. This should
be carried in your billfold or wallet. It will give
information on antibiotics that are needed during
dental or oral surgery, or if a bacterial infection
develops.
Frequently Asked Questions about Knee
Replacement Surgery
Q 1 Who is a candidate for a total
replacement?
Total knee replacements are usually
performed on people suffering from severe arthritic
conditions. Most patients whohave artificial knees
are over age 55, but the procedure is performed in
younger people.
The circumstances vary somewhat,
but generally you would be considered for a total
knee replacement if:
- You have daily pain.
- Your pain is severe enough to restrict not only
work and recreation but also the ordinary activities
of daily living.
- You have significant stiffness of your knee.
- You have significant instability (constant giving
way) of your knee.
- You have significant deformity (knock-knees or
bowlegs).
Q 2 What are the risks of total knee
replacement?
Total knee replacement is a major
operation. The most common complications are not directly
related to the knee and usually do not affect the
result of the operations. These complications include
urinary tract infection, blood clots in a leg, or
blood clots in a lung.
Complications affecting the knee are less common,
but in these cases the operation may not be as successful.
These complications include:
- Some knee pain
- Loosening of the prosthesis
- Stiffness
- Infection in the knee
A few complications such as infection,
loosening of prosthesis, and stiffness may require
reoperation. Infected artificial knees sometimes have
to be removed. This would leave a stiff leg about
one to three inches shorter than normal. However,
your leg would usually be reasonably comfortable,
and you would be able to walk with the aid of a cane
or crutches, and a shoe lift. After a course of antibiotics
the surgery can often be repeated to give a normal
knee.
Q 3 When do I return to the clinic?
Even if everything is fine, it is
advisable to return every three years after the surgery
for a review. In the meanwhile if you have any questions
or concerns please do not hesitate to write to us
at
Q 4 Should I have a total knee replacement?
Total knee replacement is an elective
operation. The decision to have the operation is not
made by the doctor, it is made by you.
All your questions should be answered
before you decide to have the operation. If you have
any questions, please feel free to write to us at
Q 5 Who develops a more severe or
an earlier arthritis?
One who has family history (this
having a strong hereditary influence), who has history
of injury in the joint (e.g. a fracture or a ligament/meniscal
injury in the knee), who has deformity of knees and
the one who is overweight. Medicines are not the treatment
for this form of arthritis. Weight reduction, regular
exercises, local heat therapy help in early stages.
Physiotherapy is the mainstay of the treatment. Painkillers
should be used only occasionally as they adversely
affect our kidneys, cause intestinal ulcers and bleeding.
Another form of Arthritis is Inflammatory arthritis
(Rheumatoid or its variants). This does need medical
treatment (DMARD's), which changes the course of the
disease and prevents further damage to joints. Surgical
treatment is needed when structural joint changes
have taken place. Before and after the surgery, the
patient should remain under care of a Physician/Rheumatologist.
Post Traumatic Arthritis can follow
a serious knee injury. A knee fracture or severe tears
of the knee's ligaments may damage the articular cartilage
over time, causing knee pain and limiting knee function.
Q 6 When can I return home?
You will be discharged when you
can get out of bed on your own and walk with a walker
or crutches, walk up and down three steps, bend your
knee 90 degrees, and straighten your knee.
Q 7 What measures should be taken
after the surgery/operation (Post operative instruction)
The success of your surgery also
will depend on how well you follow your orthopaedic
surgeon's instructions at home during the first few
weeks after surgery.
Wound Care you will have stitches
or staples running along your wound or a suture beneath
your skin on the front of your knee. The stitches
or staples will be removed several weeks after surgery.
A suture beneath your skin will not require removal.
Avoid soaking the wound in water
until the wound has thoroughly sealed and dried. A
bandage may be placed over the wound to prevent irritation
from clothing or support stockings.
Diet some loss of appetite is common
for few days after surgery. A balanced diet, often
with an iron supplement, is important to promote proper
tissue healing and restore muscle strength.
Activity Exercise is a critical
component of home care, particularly during the first
few weeks after surgery. You should be able to resume
most normal activities of daily living within three
to six weeks following surgery. Some Pain with activity
and at night is common for several weeks after surgery.
Your activity program should include:
- A graduated walking program to slowly increase
your mobility, initially in your home and later
outside.
- Resuming other normal household activities, such
as sitting and standing and walking up and down
stairs.
- Specific exercises several times a day to restore
movement and strengthen your knee. You probably
will be able to perform the exercises without help,
but you may have a physical therapist help you at
home or in a therapy center the first few weeks
after surgery.
Driving usually begins when your
knee bends sufficiently so you can enter and sit comfortably
in your car and when your muscle control provides
adequate reaction time for braking and acceleration.
Most individuals resume driving about four to six
weeks after surgery.
Q 8 What activities should I Avoid
after Knee Replacement?
Even though you may increase your
activity level after a knee replacement, you should
avoid high-demand or high-impact activities. You should
definitely avoid running or jogging, contact sports,
jumping sports, and high impact aerobics.
You should also try to avoid vigorous
walking or hiking, skiing, tennis, repetitive lifting
exceeding 50 pounds, and repetitive aerobic stair
climbing. The safest aerobic exercise is biking (stationary
or traditional) because it places very little stress
on the knee joint.
Amazon will work with you and our India
Affiliates to create a package where all your Orthopaedic
concerns/problems can be addressed. If you have any
questions, please do not hesitate to contact us by
phone or email.
|