| Spinal
Cord
Backache is the main cause of absence
from work in working population. It is also the main
presenting complaint of almost 60% of patients in
any busy orthopedic surgeon's practice. Commonest
cause of backache is "prolapsed inter-vertebral
disc" which is commonly known as slipped disc.
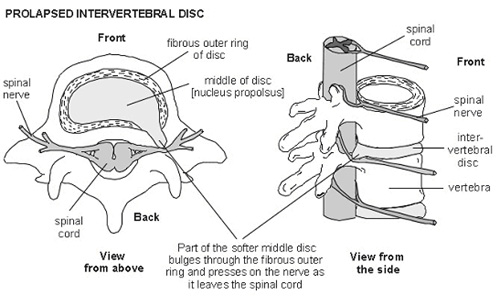
Between two vertebras there is fibro-cartilagenous
structure known as disc. Inter-vertebral disc is composed
of outer tough fibrous structure called annulus fibrosus,
which encloses jelly like structure called nucleus
pulposus. Tear of annulus forces nucleus out side,
this nucleus material which has come out presses on
the neural structures lying behind disc and causes
backache, leg pain(sciatica).
Conventional treatment of slipped
disc involves rest, physiotherapy and analgesics for
adequate period of time. However, failure of conservative
treatment, all progressive neurological deficit, and
intractable pain, surgery is required.
Conventional Spine surgery involves
taking long incisions, forceful muscle retraction
for prolonged time, removal of normal tissues like
ligaments and bone to approach area of pathology.
Most of the times these surgeries are done under prolonged
general anesthesia.
This long incisions and injury to normal
structures results in
- Increased blood loss
- Increased scar tissue formation
- Increased chance of neural injury
- Epidural scarring
- Denervation of paraspinal muscles
All these cause increased morbidity
and failed surgery syndrome. Since many times patients
require to stay in bed for long duration of time,
and there is also loss of work, earning , patients
tend to avoid surgery and prefer to suffer pain and
disability. Now there is hope for all these suffering
population, in the form of minimal invasive spine
surgery.
Minimal Invasive spine surgery involves
- Use of very small incisions,
- Minimal muscle retraction,
- Less normal tissue damage
- Targeted treatment of pathology.
Advantages:-
- Many surgeries are done under local anesthesia,
hence surgeries can be done even in patients with
high risk of anesthesia.
- There is less blood loss.
- Minimal morbidity.
- Patient can be mobilized very early and he can
be back to work faster.
- It prevents complications associated with prolonged
bed rest.
Since normal tissues are not removed
or damaged, post operative pain is less and also there
is less chance of failed back syndrome.
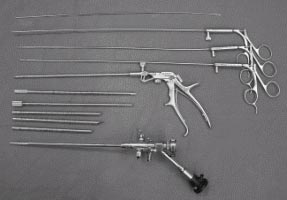
Percutaneous endoscopic lumbar discectomy
is the ultimate form of minimal invasive spine surgery.
In this form of surgery, an instrument called endoscope
is used. Whole surgery is done under local anesthesia
and patient is fully awake during surgery. In fact
for successful surgery patients active participation
is necessary.
Patient is made to lie prone on
operation table and exact entry point is mapped on
patients body using image intensifier x-ray system.
A long spinal needle is passed from side of back which
goes into disc directly by-passing other bone and
ligaments. Through this needle guide wire is passed
and after taking 5mm incision, dilator and working
cannula are passed under local anesthesia., through
which endoscope is passed. Camera and monitor is attached
to endoscope and prolapsed part of disc is removed
under vision. Wound is closed with single stitch.
Patient gets immediate pain relief and he can go home
in 24 hrs and can resume his work soon.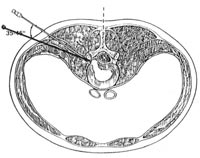
Advantages:-
- Surgery done under local anesthesia with conscious
sedation
- 5 mm skin incision
- Endoscope used for surgery
- No muscle, ligament or normal tissue damage
- Targeted fragmentectomy. (directly prolapsed
disc tissue removed.)
- Minimal blood loss
- Patient can be discharged in 24 Hrs.
- No prolonged bed rest required after surgery.
Can resume work sooner.
- Even prolapsed, migrated, extra-foraminal, recurrent
discs can be removed. Very good technique for old
and
 medically
compromised patients. medically
compromised patients.
|