| Colorectal
(Colon) Cancer
Basic Information
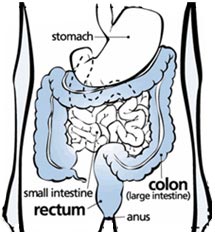 Colorectal
cancer is cancer that occurs in the colon or rectum
Sometimes it is called colon cancer, for short. As
the drawing shows, the colon is the large intestine
or large bowel. The rectum is the passageway that
connects the colon to the anus Colorectal
cancer is cancer that occurs in the colon or rectum
Sometimes it is called colon cancer, for short. As
the drawing shows, the colon is the large intestine
or large bowel. The rectum is the passageway that
connects the colon to the anus
Colorectal cancer affects both men
and women of all racial and ethnic groups, and is
most often found in people aged 50 years or older.
For men, colorectal cancer is the third most common
cancer after prostate and lung cancers. For women,
colorectal cancer is the third most common cancer
after breast and lung cancers.
Screening can find precancerous
polyps-abnormal growths in the colon or rectum-so
that they can be removed before turning into cancer.
Screening also helps find colorectal cancer at an
early stage, when treatment often leads to a cure
Symptoms
Colorectal cancer first develops with
few, if any, symptoms. However, if symptoms are present,
they may include:
- Blood in or on the stool
- A change in bowel habits
- Stools that are narrower than usual
- General, unexplained stomach discomfort
- Frequent gas, pains or indigestion;
- Unexplained weight loss
- Chronic fatigue
These symptoms can also be associated
with many other health conditions. If you have any
of these symptoms, discuss them with your doctor.
Only your doctor can determine why you're having these
symptoms.
Screening Saves Lives
Colorectal cancer almost always
develops from precancerous polyps (abnormal growths)
in the colon or rectum. Screening tests can find precancerous
polyps, so that they can be removed before they turn
into cancer. Screening tests can also find colorectal
cancer early, when treatment works best.
When Should I Begin to Get Screened?
You should begin screening for colorectal
cancer soon after turning 50, then continue getting
screened at regular intervals. However, you may need
to be tested earlier or more often than other people
if:
You or a close relative have had colorectal polyps
or colorectal cancer; or
You have inflammatory bowel disease.
Speak with your doctor about when
you should begin screening and how often you should
be tested.
What Is Colorectal Cancer Screening?
Screening is when a test is used
to look for a disease before there are any symptoms.
Cancer screening tests, including those for colorectal
cancer, are effective when they can detect disease
early. Detecting disease early can lead to more effective
treatment. In some cases, screening tests can detect
abnormalities such as polyps, before they have a chance
to turn into cancer. So removing polyps prevents colorectal
cancer from developing.
Frequently Asked Questions
What is colorectal cancer?
Cancer is a group of diseases in
which there is abnormal and uncontrolled growth of
cells in the body. If left untreated, malignant (or
cancerous) cells can spread to other parts of the
body. "Colorectal" refers to the colon and
rectum, which together make up the large intestine.
Colorectal cancer can begin anywhere in the large
intestine.
The majority of colorectal cancers
begin as polyps-abnormal growths-inside the colon
or rectum that may become cancers over a long period
of time.
What causes colorectal cancer?
The exact cause of most colorectal
cancers is not yet known. About 75% of colorectal
cancers occur in people with no known risk factors.
There are some known factors that may increase a person's
risk of developing colorectal cancer, which include:
A personal or family history of colorectal polyps
or colorectal cancer;
Inflammatory bowel disease (ulcerative colitis or
Crohn's disease); or
Genetic syndromes such as familial adenomatous polyposis
(FAP) or hereditary nonpolyposis colon cancer (HNPCC).
(Just 5% of colorectal cancers are linked to these
genetic syndromes.)
What are the symptoms of colorectal
cancer?
Colorectal cancer first develops with
few, if any, symptoms. However, if symptoms are present,
they may include:
- Blood in or on the stool;
- A change in bowel habits;
- Stools that are narrower than usual;
- General, unexplained stomach discomfort;
- Frequent gas, pains or indigestion;
- Unexplained weight loss; and
- Chronic fatigue.
These symptoms can also be associated
with many other health conditions. If you have any
of these symptoms, discuss them with your doctor.
Only your doctor can determine why you're having these
symptoms.
Who is at risk of developing colorectal
cancer?
Colorectal cancer occurs in men
and women of all racial and ethnic groups. Approximately
75% of colorectal cancers occur in people with no
known risk factors. Other important facts about risk
for colorectal cancer include:
- More than 90% of colorectal cancers are diagnosed
in people aged 50 or older. The risk of developing
colorectal cancer increases with age.
- A family history of colorectal cancer or colorectal
polyps may increase a person's risk of developing
colorectal cancer.
- Certain diseases of the intestines, including
inflammatory bowel disease (ulcerative colitis or
Crohn's disease), can increase the risk for colorectal
cancer.
Is there anything I can do to reduce
my risk for colorectal cancer?
There is strong scientific evidence
that having regular screening tests for colorectal
cancer beginning at age 50 reduces deaths from colorectal
cancer. Screening tests can find precancerous polyps
(abnormal growths) in the colon and rectum, and polyps
can be removed before they turn into cancer.
Studies have also shown that increased
physical activity and maintaining a healthy weight
can decrease the risk for colorectal cancer. Evidence
is less clear about other ways to prevent colorectal
cancer.
Research is underway to determine
whether dietary changes may decrease the risk for
colorectal cancer. Currently, there is no consensus
on the role of diet in preventing colorectal cancer;
however, medical experts recommend a diet low in animal
fats and high in fruits, vegetables, and whole grain
products to reduce the risk of other chronic diseases,
such as coronary artery disease and diabetes. This
diet also may reduce the risk of colorectal cancer.
In addition, researchers are examining
the role of certain medications and supplements, including
aspirin, calcium, vitamin D, and selenium, in preventing
colorectal cancer. Overall, the most effective way
to reduce your risk of colorectal cancer is by having
regular colorectal cancer screening tests beginning
at age 50.
What is colorectal cancer screening?
Screening is when a test is used
to look for a disease before there are any symptoms.
Cancer screening tests, including those for colorectal
cancer, are effective when they can detect disease
early. Detecting disease early can lead to more effective
treatment. In some cases, screening tests can detect
abnormalities such as polyps before they have a chance
to turn into cancer. So removing polyps can prevent
colorectal cancer from developing.
What are the screening tests for colorectal
cancer?
Several tests are available to screen
for colorectal cancer. Some are used alone; others
are used in combination with each other. Talk with
your doctor about which test or tests are best for
you.
Fecal Occult Blood Test (FOBT)-
This test checks for occult (hidden) blood in the
stool. At home, you place a small amount of your stool
from three consecutive bowel movements on test cards.
You return the cards to your doctor's office or a
lab where they're checked for blood. This test is
recommended yearly. (If blood is found, you will need
a follow-up colonoscopy.)
Flexible Sigmoidoscopy- Before this
test, you use a strong laxative and/or enema to clean
out the colon. Flexible sigmoidoscopy is conducted
in a doctor's office, clinic, or hospital. The doctor
(or other specially-trained healthcare professional)
uses a narrow, flexible, lighted tube to look at the
inside of the rectum and the lower portion of the
colon. During the exam, the doctor may remove polyps
(abnormal growths) and collect samples of tissue or
cells for closer examination. This test is recommended
every five years. (If polyps are found, you will need
a follow-up colonoscopy.)
Combination of FOBT and Flexible
Sigmoidoscopy- Some doctors recommend having both
FOBT and flexible sigmoidoscopy to increase the chance
of finding polyps and cancers. When used in combination,
FOBT is recommended yearly and flexible sigmoidoscopy
is recommended every five years.
Colonoscopy- Before this test, you
take a strong laxative to clean out the colon. Colonoscopy
is conducted in a doctor's office, clinic, or hospital.
You are given a sedative to make you more comfortable
while the doctor uses a narrow, flexible, lighted
tube to look at the inside of the rectum and the entire
colon. This test is similar to flexible sigmoidoscopy,
except the tube used is longer and allows the doctor
to see the entire colon. During the exam, the doctor
may remove polyps and collect samples of tissue or
cells for closer examination. This test is recommended
every 10 years. (Colonoscopy also is used as a follow-up
test if anything unusual is found during one of the
other screening tests.)
Double-Contrast Barium Enema- This
test is conducted in a radiology center or hospital.
Before the test, you use a strong laxative and/or
enema to clean out the colon. For this procedure,
you are given an enema with a barium solution, followed
by an injection of air. An X-ray of the rectum and
colon is then taken. The barium coats the lining of
the intestines so that polyps and other abnormalities
are visible on the X-ray. This test is recommended
every five years. (If polyps are found, you will need
a follow-up colonoscopy.)
Who should be tested for colorectal
cancer?
All men and women aged 50 years
and older should be tested for colorectal cancer routinely.
Others who are at increased risk should speak to their
doctors about earlier or more frequent testing. Those
at increased risk are people with:
A family history of colorectal cancer or colorectal
polyps;
Certain diseases of the intestines, including inflammatory
bowel disease (ulcerative colitis or Crohn's disease);
or
Genetic syndromes such as familial adenomatous polyposis
(FAP) or hereditary nonpolyposis colon cancer (HNPCC).
(Just 5% of colorectal cancers are linked to these
genetic syndromes).
What about testing for colorectal
cancer using newer technology, such as virtual colonoscopy,
fecal immunochemical testing (FIT or iFOBT), and stool
DNA testing?
Although virtual colonoscopy and
stool DNA testing are used in some medical settings,
data are not yet sufficient to support these tests
for colorectal cancer screening. Research is underway
to evaluate their effectiveness as screening tests,
especially compared with the screening tests already
recommended for colorectal cancer.
Virtual colonoscopy, also called
computed tomographic (CT) colonography, uses multiple
CT images to create a three-dimensional view of the
colon. As is the case with traditional colonoscopy,
a patient must prepare for virtual colonoscopy by
drinking a strong laxative to clean out the colon
thoroughly.
During virtual colonoscopy, air
is pumped into the rectum to expand the rectum and
colon. If a polyp or other abnormality is found, it
cannot be removed during this procedure. A follow-up
colonoscopy will be necessary to remove polyps or
take tissue samples for further analysis. Because
virtual colonoscopy is still considered experimental,
most insurance plans do not cover the procedure.
The fecal immunochemical test (FIT
or iFOBT) is a newer kind of stool blood test kit.
It detects occult (hidden) blood in the stool. This
test is done essentially the same way as FOBT, but
is more specific and has fewer false positive results.
Vitamins and foods do not affect this test, so dietary
restrictions are not necessary. As with FOBT, the
FIT may not detect a tumor that is not bleeding, and
you will need to have a colonoscopy if the test results
show there is hidden blood in the stool. Organizations
that issue screening guidelines are studying when
and if to add FIT to the recommendations.
Molecular testing of genetic material
(DNA) in stool is another promising technology that
may become an option for screening in the future.
This technique has not yet been shown to detect precancerous
polyps and is still experimental.
Why should I get screened for colorectal
cancer?
Screening saves lives. Colorectal
cancers almost always develop from precancerous polyps
(abnormal growths) in the colon or rectum. Screening
tests can find polyps, so they can be removed before
they turn into cancer. Screening tests also can find
colorectal cancer early, when treatment works best
and the chance for a full recovery is very high.
Having regular screening tests beginning
at age 50 could save your life.
How do I know which screening test
is right for me?
Scientific data do not currently
suggest that there is a single "best test"
for any one person. Each test has advantages and disadvantages.
Patients and their doctors are encouraged to discuss
the benefits and potential risks associated with each
screening option as they decide which test to use
and how often the patient should be tested. Which
test to use will depend on:
A patient's preferences;
A patient's medical condition;
The likelihood that the patient will have the test;
and
The resources available for testing and follow-up.
Is colorectal cancer screening covered
by insurance?
Most insurance plans help pay for
screening tests for people aged 50 or older. Many
plans also help pay for screening tests for people
less than age 50 who are at increased risk for colorectal
cancer. Check with your health insurance provider
to determine your colorectal cancer screening benefits.
|



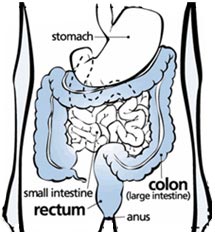 Colorectal
cancer is cancer that occurs in the colon or rectum
Sometimes it is called colon cancer, for short. As
the drawing shows, the colon is the large intestine
or large bowel. The rectum is the passageway that
connects the colon to the anus
Colorectal
cancer is cancer that occurs in the colon or rectum
Sometimes it is called colon cancer, for short. As
the drawing shows, the colon is the large intestine
or large bowel. The rectum is the passageway that
connects the colon to the anus