| Ovarian
Cancer
Basic Information
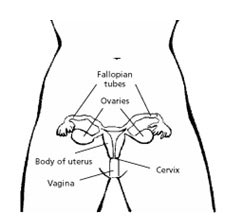 Ovarian cancer is cancer that begins in the ovaries. One ovary
is located on each side of your uterus in the pelvis.
They are each connected to the uterus through the
fallopian tube, the tube through which the eggs travel
to be fertilized in the uterus (womb).
Ovarian cancer is cancer that begins in the ovaries. One ovary
is located on each side of your uterus in the pelvis.
They are each connected to the uterus through the
fallopian tube, the tube through which the eggs travel
to be fertilized in the uterus (womb).
The ovaries contain three kinds
of tissue. Ovaries contain germ cells cells that produce
eggs (ova) that are formed on the inside of the ovary.
Each month from puberty until menopause, women normally
produce an egg that makes its way to the surface,
where it is shed into the fallopian tube. The ovaries
also contain cells, called stromal cells, which produce
most of the female hormones, estrogen and progesterone.
A layer of tissue called epithelium covers the ovary.
Most ovarian cancers start in this epithelial covering.
Because ovarian epithelial cancers
arise from cells on the surface of the ovary, they
tend to spread throughout the pelvis and abdomen,
even when the tumor is small. Cancer cells break off
from the tumor surface and circulate through the abdominal
cavity, where they can implant and begin growing.
They can circulate as far up as the underside of the
diaphragm, the muscle that separates the lungs from
the abdomen. They also can spread to the omentum,
an apron of fatty tissue that covers the intestines.
Because the ovary is richly supplied
with lymphatic vessels, the cancer cells also tend
to migrate into the lymph nodes that cluster around
the aorta. Lymphatic vessels are similar to veins
except they are thinner and more delicate and carry
clear lymph fluid. Lymph nodes are small bean-shaped
collections of immune cells that fight infection.
The aorta runs along the back of the abdomen.
Types of Ovarian Cancer
There are several types of ovarian
cancer, but this website discusses only epithelial
ovarian tumors.
Benign epithelial ovarian tumors
Most epithelial ovarian tumors are
benign, do not spread, and usually do not lead to
serious illness. There are several types of benign
epithelial tumors, including serous adenomas, mucinous
adenomas, and Brenner tumors.
Tumors of low malignant potential:
When viewed under the microscope, some ovarian epithelial
tumors do not clearly appear to be cancerous. These
are called tumors of low malignant potential (LMP
tumors). They are also known as borderline epithelial
ovarian cancer. These differ from typical ovarian
cancers in that they do not invade the ovarian stroma
(the supporting tissue of the ovary). Likewise, if
they spread outside the ovary, for example, into the
abdominal cavity, they do not usually invade the lining
tissue of the abdomen.
These cancers affect women at a
younger age than the typical epithelial ovarian cancers.
LMP tumors grow slowly and are also a less life-threatening
disease than most ovarian cancers. Although they can
be fatal, this is not common. Because of this, LMP
tumors are treated differently, and a separate treatment
pathway is presented in this report.
Epithelial ovarian cancers
Cancerous epithelial tumors are
called carcinomas. About 85% of ovarian cancers are
epithelial ovarian carcinomas. Epithelial ovarian
carcinoma cells have several features that can be
identified under the microscope. These features are
used to classify epithelial ovarian carcinomas into
serous, mucinous, endometrioid, and clear cell types.
Although these cancers may grow a little differently,
they are all treated the same way.
Undifferentiated epithelial ovarian
carcinomas don't look like any of these four subtypes,
and they also tend to grow and spread more quickly.
In addition to their classification by cell type,
epithelial ovarian carcinomas are also given a grade
and a stage. The staging system is described in the
staging section.
The grade is on a scale of 1, 2,
or 3. Grade 1 epithelial ovarian carcinomas more closely
resemble normal tissue, grow more slowly, and tend
to have a better prognosis (outlook for survival).
Grade 3 epithelial ovarian carcinomas less closely
resemble normal tissue, are more aggressive, and usually
have a worse outlook.
The tumor stage describes how far
the tumor has spread from where it started in the
ovary.
What Causes Ovarian Cancer?
A risk factor is anything that increases
a person's chance of getting a disease such as cancer.
Different cancers have different risk factors. For
example, unprotected exposure to strong sunlight is
a risk factor for skin cancer. Smoking is a risk factor
for cancers of the lung, mouth, larynx, bladder, kidney,
and several other organs.
Researchers have discovered several
specific factors that increase a woman's likelihood
of developing epithelial ovarian cancer. These risk
factors do not apply to other less common types of
ovarian cancer, such as germ cell tumors and stromal
tumors.
Most women with ovarian cancer do
not have any known risk factors. It is important to
remember that risk factors increase the odds of getting
a disease but do not guarantee it will occur. Only
a small number of women who have risk factors will
develop ovarian cancer.
Aging
Most ovarian cancers develop after
menopause. A woman is considered menopausal when she
has gone a year without a menstrual period. Half of
all ovarian cancers are found in women over the age
of 63.
Reproductive history
Women who started menstruating at
an early age (before age 12), had no children or had
their first child after age 30, and/or experienced
menopause after age 50 may have an increased risk
of ovarian cancer. A relationship seems to exist between
the number of menstrual cycles in a woman's lifetime
and her risk of developing ovarian cancer.
Fertility drugs
The use of the fertility drug clomiphene
citrate over several years, especially without getting
pregnant, may increase your risk for developing ovarian
tumors, particularly a type known as borderline epithelial
ovarian cancer (or tumors of low malignant potential).
If you are taking this drug, you should discuss its
potential risks with your doctor. However, infertility
also increases the risk of ovarian cancer, even without
use of fertility drugs.
Family history of ovarian cancer,
breast cancer, or colorectal cancer: Ovarian cancer
risk is increased if your mother, sister, or daughter
have, or have had, ovarian cancer, especially if they
developed ovarian cancer at a young age. You can inherit
an increased risk for ovarian cancer from relatives
on your mother's side or father's side of the family.
About 10% of ovarian cancers result from an inherited
tendency to develop the disease. If there is a family
history of cancer due to an inherited mutation of
the breast cancer gene BRCA1 or BRCA2, you will have
a very high risk of ovarian cancer. Also, a mutation
leading to inherited colorectal cancer can also lead
to ovarian cancer. Many cases of familial epithelial
ovarian cancer are caused by inherited gene mutations
that can be identified by genetic testing.
Breast cancer
If you have had breast cancer, you
also have an increased risk of developing ovarian
cancer. There are several reasons for this. Some of
the reproductive risk factors for ovarian cancer may
also increase breast cancer risk. Also, if you have
a strong family history of breast cancer, you may
have an inherited mutation of the BRCA1 or BRCA2 gene.
Talcum powder
It has been suggested that talcum
powder applied directly to the genital area or on
sanitary napkins may be carcinogenic (cancer-causing)
to the ovaries. Most but not all studies suggest a
slight increase in risk of ovarian cancer in women
who used talc on the genital area. In the past, talcum
powder was sometimes contaminated with asbestos, a
known cancer-causing mineral. This may explain the
association with ovarian cancer in some studies. Body
and face powder products have been required by law
for more than 20 years to be asbestos-free. However,
proving the safety of these newer products will require
follow-up studies of women who have used them for
many years. There is no evidence at present linking
cornstarch powders with any female cancers.
Hormone replacement therapy
Some studies suggest that women
using estrogens after menopause may have a slightly
increased risk of developing ovarian cancer, while
other studies have not found any effect on ovarian
cancer risk. A recent study suggested that women using
estrogens for more than 10 years almost doubled their
ovarian cancer risk. The decision to use hormone replacement
therapy (HRT) after menopause should be made by a
woman and her doctor after weighing the possible risks
and benefits. Factors to consider include other risk
factors for ovarian cancer, breast cancer, osteoporosis
(thinning and weakening of bones), and the severity
of menopausal symptoms.
Can Ovarian Cancer Be Prevented?
Most women have one or more risk
factors for ovarian cancer. However, most of the common
factors only slightly increase your risk, so they
only partly explain the frequency of the disease.
So far, knowledge about risk factors has not been
translated into practical ways to prevent most cases
of ovarian cancer.
There are several ways you can reduce
your risk of developing epithelial ovarian cancer.
However, some of these strategies reduce the risk
only slightly, while others decrease it much more.
Some strategies are easily followed, and others require
surgery. If you are concerned about your risk of ovarian
cancer, you may want to discuss this information with
your health care team.
Oral contraceptives
The use of oral contraceptives (birth
control pills) decreases the risk of developing ovarian
cancer, especially among women who used them for several
years. It is unclear if oral contraceptives reduce
the ovarian cancer risk in women who have the BRCA1
or BRCA2 gene mutation.
Tubal ligation or hysterectomy
Tubal ligation is a surgical procedure
to "tie" the fallopian tubes to prevent
pregnancy. When performed after childbearing, tubal
ligation may reduce the chance of developing ovarian
cancer. A hysterectomy may also reduce your risk.
Pregnancy and breast-feeding
Having one or more children, particularly
if your first child is born before you are age 30,
plus prolonged (one year or more) breast-feeding also
may decrease your risk. Although these measures slightly
reduce risk, they do not guarantee protection against
ovarian cancer. Doctors do not recommend making choices
about when to have a child specifically for the purpose
of reducing ovarian cancer risk, especially since
using oral contraceptives has a greater impact on
this risk.
Diet
Results of some studies suggest
that a high-fat diet may increase ovarian cancer risk.
Prevention strategies for women with
a family history of ovarian cancer
Genetic counseling can predict whether
you are likely to have one of the gene mutations associated
with an increased ovarian cancer risk. If your family
history suggests that you might have one of these
gene mutations, genetic testing can be done.
Before undergoing genetic testing,
you should discuss its benefits and potential drawbacks.
Genetic testing can determine if you or members of
your family carry certain gene mutations that cause
a high risk of ovarian cancer. For some women with
a strong family history of ovarian cancer, knowing
that they do not have a mutation that increases their
ovarian cancer risk can be a great relief for them
and their children. Knowing that you do have such
a mutation can be very stressful, but many women find
this information helpful in making important decisions
about certain prevention strategies for them and their
children.
Use of oral contraceptives is one
way to decrease ovarian cancer if you are at high
risk for this disease. However, some studies have
indicated that oral contraceptives might increase
your breast cancer risk if you have a strong family
history of breast cancer. Other studies, on the other
hand, have not found any increase in breast cancer
risk among women with BRCA mutations who take oral
contraceptives. Additional research is needed to learn
more about the risks and benefits of oral contraceptives
for women at high ovarian and breast cancer risk.
A prophylactic oophorectomy is surgery
to remove both of the ovaries before an ovarian cancer
occurs. This is a controversial operation because
it causes premature menopause in premenopausal women
and may be unnecessary. It generally is recommended
only for certain very high-risk patients over age
40. This operation lowers ovarian cancer risk a great
deal but does not entirely eliminate it. In some women
with a very high risk of ovarian cancer (due to a
strong family history) who have had both ovaries removed,
cancers can still form in the lining cells of the
pelvic cavity where the ovaries were previously located.
This type of cancer, known as primary peritoneal carcinoma,
occurs more often in women with BRCA gene mutations.
Recent studies suggest that having both ovaries removed
can also lower the risk of developing breast cancer
among women with BRCA gene mutations.
As noted in the section on known
risk factors for ovarian cancer, risk gene mutations
and women with a strong family history who have not
undergone genetic testing may benefit from screening
tests.
Finding Ovarian Cancer Early
About 25% of ovarian cancers are
found at an early stage. Early detection improves
the chances that ovarian cancer can be treated successfully.
When ovarian cancer is found early at a localized
stage, about 90% of patients live longer than 5 years
after diagnosis.
Regular pelvic examinations
Yearly pelvic examinations and Pap
smears to check the pelvic area should begin at age
18 or when you become sexually active, whichever comes
first. During this exam, the health care professional
feels the ovaries and uterus for size, shape, and
consistency.
Although the Pap test is effective
in detecting cervical cancer early, it cannot detect
most ovarian cancers. Most of the ovarian cancers
that are detected through Pap smears are already advanced.
Although a pelvic examination is routinely recommended
because it can find some reproductive system cancers
at an early stage, most early ovarian tumors are difficult
or impossible for even the most skilled examiner to
feel.
Seeing a doctor if you have symptoms:
Early cancers of the ovaries tend to cause symptoms
that are relatively vague. These symptoms include
abdominal swelling (due to a mass or accumulation
of fluid), unusual vaginal bleeding, pelvic pressure,
back pain, leg pain, and digestive problems such as
gas, bloating, indigestion, or long-term stomach pain.
Most of these symptoms can also be caused by other
less serious conditions.
By the time ovarian cancer is considered
as a possible cause of these symptoms, it may have
already spread beyond the ovaries. Also, ovarian cancer
can rapidly spread to the surface of nearby organs.
Nonetheless, prompt attention to symptoms can improve
the odds of early diagnosis and successful treatment.
If you have symptoms of ovarian cancer, report them
to your health care professional right away.
Screening tests for ovarian cancer:
Screening tests and examinations are used to detect
a disease, such as cancer, in people who do not have
any symptoms. Women with a high risk of developing
epithelial ovarian cancer, such as those with a very
strong family history of this disease, may be screened
with transvaginal sonography (an ultrasound test performed
with a small instrument placed in the vagina) and
blood tests.
Transvaginal sonography is helpful
in finding a mass in the ovary, but it does not accurately
detect which masses are cancers and which are benign
diseases of the ovary.
Blood tests for ovarian cancer may
include measuring the amount of CA-125. The amount
of this protein in the blood is higher in many women
with ovarian cancer. However, some noncancerous diseases
of the ovaries can also increase the blood levels
of CA-125, and some ovarian cancers may not produce
enough CA-125 to cause a positive test result. When
these test results are positive, it may be necessary
to do more x-ray studies or to take samples of fluid
from the abdomen or tissue from the ovaries to find
out if a cancer is really present.
In preliminary studies of women
at average risk of ovarian cancer, these screening
tests did not lower the number of deaths caused by
ovarian cancer. Therefore, transvaginal sonography
and the CA-125 blood test are not recommended for
ovarian cancer screening of women without known strong
risk factors. Researchers continue to study ways to
improve ovarian cancer screening tests. They hope
that further improvements will make these tests effective
enough to lower the ovarian cancer death rate.
Tests and Exams to Diagnose Ovarian
Cancer
If there is a reason to suspect
that you may have ovarian cancer, the doctor will
use one or more methods to find out if the disease
is really present. If these tests find ovarian cancer,
more tests will be done to find out how far the cancer
has spread.
History and Physical Exam
When your doctor "takes a history,"
he or she will ask you a series of questions about
your symptoms and risk factors. Ovarian cancer may
cause several signs and symptoms. However, most of
these may also be caused by benign (noncancerous)
diseases and by cancers of other organs.
Prolonged swelling of the abdomen (due to a tumor
or accumulation of fluid called ascites) Digestive
problems including gas, loss of appetite, bloating,
long-term abdominal pain, or indigestion
Unusual vaginal bleeding is a rare sign of ovarian
cancer. It is a strong warning of some type of abnormality,
although not necessarily ovarian cancer. Bleeding
that occurs between periods, is heavier, or lasts
longer than usual is considered abnormal. Any postmenopausal
bleeding, staining, or persistent vaginal discharge
is abnormal. A woman of any age who has unusual vaginal
bleeding should tell her doctor immediately.
Pelvic pressure (feeling as though you have to urinate
or defecate all the time)
Pelvic pain is a nonspecific symptom. It may be caused
by ovarian cancer, other cancers, or by several benign
conditions.
Leg pain
Back pain
If ovarian cancer is suspected,
your doctor will use one or more methods to be absolutely
certain that the disease is present and to determine
the stage of the cancer.
Consultation with a Specialist
If your pelvic examination or other
tests suggest that you may have ovarian cancer, you
will need a doctor or surgeon who specializes in treating
women with this type of cancer. A gynecologic oncologist
is a doctor who is specially trained in treating cancers
of the female reproductive system.
Blood Tests
Certain blood tests are useful in
evaluating ovarian cancer. The simplest is a complete
blood count (CBC). This tests for anemia (from too
few red blood cells), which could be the result of
internal bleeding. It also tests whether you are producing
normal numbers of infection-fighting white blood cells
and platelets (blood particles that help prevent bleeding).
A second test is a general blood chemistry test. This
tells about your liver and kidney function and your
blood mineral balance.
Your doctor will also perform a
blood CA-125 test. CA-125 is a tumor marker, a substance
that is elevated in the blood of many women with ovarian
cancer. It is often very high when the cancer is advanced.
After treatment, it will return to normal levels if
the cancer goes into remission or if it is completely
removed by surgery.
Imaging Studies
Imaging methods such as computed
tomography (CT) scans, magnetic resonance imaging
(MRI) studies can confirm whether a pelvic mass is
present. Although these studies cannot confirm if
the mass is a cancer, they are useful if your doctor
is looking for spread of ovarian cancer to other tissues
and organs.
Ultrasound
An ultrasound uses sound waves to
create an image on a video screen. Sound waves are
released from a small probe placed in the woman's
vagina or on the surface of her abdomen. The sound
waves create echoes as they enter the ovaries and
other organs. The same probe detects the echoes that
bounce back, and a computer translates the pattern
of echoes into a picture. Because ovarian tumors and
normal ovarian tissue often reflect sound waves differently,
this test may be useful in detecting tumors and in
determining whether a mass is solid or a fluid-filled
cyst.
Computed tomography (CT)
The CT scan is an x-ray procedure
that produces detailed cross-sectional images of your
body. Instead of taking one picture, as does a usual
chest x-ray, a CT scanner takes many pictures as it
rotates around you. A computer then combines these
pictures into an image of a slice of your body. The
machine produces multiple images of the part of your
body that is being studied.
Often after the first set of pictures
is taken you will receive an intravenous injection
of a contrast agent, or dye, which helps better outline
structures in your body. A second set of pictures
is then taken. Some people get hives or, rarely, more
serious allergic reactions like trouble breathing
and low blood pressure can occur. Be sure to tell
the doctor if you have ever had a reaction to any
contrast material used for x-rays. The CT scan provides
precise information about the size, shape, and position
of a tumor and can help find enlarged lymph nodes
that might contain cancer that has spread from the
ovary. Although large lymph nodes seen in CT scans
of a person with ovarian cancer usually contain cancer
cells, they may sometimes be enlarged for other reasons.
CT scans can also be used during
a biopsy to precisely guide a biopsy needle into a
suspected tumor. For this procedure, called a CT-guided
needle biopsy, the patient remains on the CT scanning
table, while a radiologist advances a biopsy needle
toward the location of the mass. CT scans are repeated
until the doctors are confident that the needle is
within the mass. A fine needle biopsy sample (tiny
fragment of tissue) or a core needle biopsy sample
(a thin cylinder of tissue about 1/2-inch long and
less than 1/8-inch in diameter) is removed and examined
under a microscope.
Magnetic resonance imaging (MRI)
MRI scans use radio waves and strong
magnets instead of x-rays. The energy from the radio
waves is absorbed and then released in a pattern formed
by the type of tissue and by certain diseases. A computer
translates the pattern of radio waves given off by
the tissues into very detailed cross-sectional images
of parts of the body. A contrast material might be
injected just as with CT scans.
Chest x-ray
This procedure may be done to determine
whether ovarian cancer has spread (metastasized) to
the lungs. This spread may cause tumors to appear
in the lungs and often causes fluid to collect around
the lungs. This fluid, called a pleural effusion,
can be seen with chest x-rays.
Barium enema x-ray
This is a test to see if the cancer
has invaded your colon (large intestine) or rectum
(it is also used to look for colorectal cancer). After
taking laxatives the day before, the radiology technician
introduces barium sulfate, a chalky substance, into
your rectum and colon. Because barium is impermeable
to x-rays, it outlines your colon and rectum on x-rays
of your abdomen.
Colonoscopy
A colonoscopy is also done after
you have cleaned out your large intestine with laxatives.
A doctor inserts a fiberoptic tube into your rectum
and passes it through your entire colon. This allows
the doctor to see the inside and detect any cancer
growing in the colon. It is also used to look for
colorectal cancer. Because this is uncomfortable,
you will be sedated. Other Tests
Laparoscopy
This procedure uses a thin, lighted
tube through which a doctor can view the ovaries,
other pelvic organs, and tissue in the area around
the bile duct. The tube is inserted through a small
incision (cut) in the lower abdomen. Laparoscopy provides
a view of organs that can help in planning surgery
or other treatments and can help doctors confirm the
stage (how far the tumor has spread) of the cancer.
Also, doctors can manipulate small instruments through
the laparascopic incision(s) to remove small tissue
samples to examine under the microscope.
Tissue Sampling (Biopsy)
The only way to determine for certain
if a growth in the pelvic region is cancer is to remove
a sample of tissue from the suspicious area and examine
it under a microscope. This procedure is called a
biopsy.
Although in many cancers a biopsy
is often done before surgery, in women with ovarian
cancer, the cancer sampling generally occurs at the
time of surgery. Not only is the entire ovary removed
for examination, but the surgeon also removes any
other visible cancer than can be removed and performs
other biopsies. Ovarian cancer tends to "seed"
throughout the abdomen and to the surface of other
organs, such as the liver. Often the surgeon can't
tell this has happened without a biopsy. The surgeon
will try to find out if or how extensively the cancer
has seeded by removing small amounts of normal appearing
tissue from many sites in the abdomen. The pathologist
then examines these under the microscope. This is
part of the "staging" procedure for ovarian
cancer. Sometimes, in patients with ascites (collection
of fluid inside the abdomen), samples of fluid can
also be used to diagnose the cancer.
Ovarian Cancer Stages
Staging is the process of finding
out how far a cancer has spread. Most ovarian cancers
that are not obviously widespread are staged at the
time of surgery. Although your doctor may try to estimate
the stage of your cancer from the examination and
imaging tests (called the clinical stage), this is
not always accurate. The pathologic stage, which is
assessed during and after surgery, is much more important.
Samples of tissues are taken from
different parts of the pelvis and abdomen and examined
under the microscope. Staging is very important because
ovarian cancers have a different prognosis at different
stages and are treated differently. The accuracy of
the staging may determine treatment and can help predict
whether a patient will be cured. If the cancer is
not properly staged, then cancer that has spread outside
the ovary may be missed and not treated. Once a stage
has been assigned, it does not change, even when the
cancer recurs or spreads to new locations in the body.
Ask your cancer care team to explain
the staging procedure. Also ask them if they will
perform a thorough staging procedure. After surgery,
ask about the stage of your cancer so that you can
take part in making informed decisions about your
treatment. The stages described below are pathologic
stages, not clinical (from physical examination and
imaging studies). They are developed from the pathologist's
report of the findings from your surgery.
What are the Stages of Ovarian Cancer
Mean
Ovarian cancer is staged using the
AJCC and FIGO system. AJCC stands for American Joint
Committee on Cancer and FIGO stands for International
Federation of Gynecologists and Obstetricians.
Stage I
The cancer is still contained within
the ovary (or ovaries).
Stage IA : Cancer
has developed in one ovary and has not spread onto
the outer surface of the ovary. Laboratory examination
of washings from the abdomen and pelvis did not find
any cancer cells.
Stage IB : Cancer
has developed within both ovaries and has not spread
onto their outer surfaces. Laboratory examination
of washings from the abdomen and pelvis did not find
any cancer cells.
Stage IC : The
cancer is present in one or both ovaries and one or
more of the following are present:
Cancer is found on the outer surface of at least one
of the ovaries.
In the case of cystic (fluid-filled) tumors, the capsule
(outer wall of the tumor) has ruptured (burst).
Laboratory examination found cancer cells in fluid
or washings from the abdomen.
Stage II
The cancer is in one or both ovaries
and has grown onto or into other organs (such as the
uterus, fallopian tubes, bladder, the sigmoid colon,
or the rectum) within the pelvis.
Stage IIA : The
cancer has spread onto or has grown into the uterus
or the fallopian tubes, or both. Laboratory examination
of washings from the abdomen did not find any cancer
cells.
Stage IIB : The
cancer has spread onto or grown into other nearby
pelvic organs, such as the bladder, the sigmoid colon,
or the rectum. Laboratory examination of fluid from
the abdomen did not find any cancer cells.
Stage IIC : The
cancer has spread onto or grown into pelvic organs
as in stages IIA or IIB, and cancer cells were found
in fluid or washings from the abdomen.
Stage III
The cancer involves one or both
ovaries, and one or both of the following are present:
Cancer has spread beyond the pelvis to the lining
of the abdomen.
Cancer has spread to lymph nodes (glands that fight
infection and produce some types of blood cells).
Stage IIIA : During
the staging operation, the surgeon can see cancer
in the ovary or ovaries but no other sites of disease
outside the ovaries are visible. However, when the
staging biopsies are checked under a microscope, tiny
deposits of cancer are found in the lining of the
abdomen. The cancer has not spread to lymph nodes.
Stage IIIB : There
is cancer in one or both ovaries, and deposits of
cancer large enough for the surgeon to see but smaller
than 2 cm (about 3/4-inch) across are present in the
abdomen. Cancer has not spread to the lymph nodes.
Stage IIIC : The
cancer is in one or both ovaries, and one or both
of the following is present:
Cancer has spread to lymph nodes.
Deposits of cancer larger than 2 cm (about 3/4 -inch)
across are seen in the abdomen.
Stage IV
This is the most advanced stage
of ovarian cancer. The cancer has spread to distant
sites such as the inside of the liver (the outside
can still be stage III), the lungs, or to other organs
located outside of the pelvis or abdomen. Finding
ovarian cancer cells in pleural fluid (from around
the lungs) is also evidence of stage IV disease.
Recurrent ovarian cancer
This means that the disease has
recurred (come back) after completion of treatment.
After the diagnostic tests are done,
your cancer care team will recommend one or more treatment
options. Consider the options without feeling rushed.
If there is anything you do not understand, ask to
have it explained. The choice of treatment depends
largely on the type of cancer and the stage of the
disease. In patients who did not have surgery as their
initial treatment, the exact stage may not be known.
Treatment then is based on other available information.
Other factors that could play a
part in choosing the best treatment plan might include
your general state of health, whether you plan to
have children, and other personal considerations.
Age alone is not a determining factor since several
studies have shown that older women tolerate ovarian
cancer treatments well. Be sure you understand all
the risks and side effects of the various therapies
before making a decision about treatment.
The main treatments for ovarian
cancer are surgery, chemotherapy, and radiation therapy.
In some cases, two or even all of these treatments
will be recommended.
Be aware that almost all the treatments
make a woman infertile, that is, unable to bear children.
If surgery is chosen, most of the time the surgeon
removes both ovaries and the uterus. This will result
in your not being able to get pregnant, and it will
also result in menopause. Both radiation and chemotherapy
also cause infertility. If you want to maintain your
fertility so that you can have a family after recovering
from treatment, discuss this with your doctor. Certain
situations in which this is possible are mentioned
later in the treatment decision tree.
Surgery
Surgery for ovarian cancer is done
for three reasons. The first is to make the diagnosis
of ovarian cancer. The second is to stage the disease.
And the third, is to remove as much of the cancer
as can be removed (this is called debulking).
Staging and removal of the ovarian
cancer are specialized procedures that require the
expertise of a gynecologic surgical oncologist who
is trained in these procedures. If ovarian cancer
is suspected before surgery, a gynecologic oncologist
should do the surgery or should be available to assist
the doctor doing the surgery.
How much surgery you have depends
on how far your cancer has spread and on your general
health. For women of childbearing age who have certain
kinds of tumors and whose cancer is in the early stage,
an effort will be made to treat the disease without
removing both ovaries and the uterus.
Almost always, the surgeon makes
a vertical incision in the abdomen. Many surgeries
on women's pelvic organs can be done with a laparoscope.
This means operating through small incisions and viewing
the organs with a telescope-like instrument. This
is not usually done for ovarian cancer. But, it may
be done in some women with stage I cancers.
Several surgical procedures are
used to treat ovarian cancer. The medical term for
these operations is based on the Greek or Latin names
of the organs they remove. The medical name of an
operation that removes something usually ends with
"-ectomy." So, removing the uterus is a
hysterectomy, removing the omentum is an omentectomy,
and removing lymph nodes is a lymphadenectomy (also
called lymph node biopsy or dissection).
There are two ovaries and two fallopian
tubes. Removing one ovary is a unilateral (one side)
oophorectomy, and removing both is a bilateral (two
sides) oophorectomy. Likewise, removing one or two
fallopian tubes is a unilateral salpingectomy or bilateral
salpingectomy. Often, several organs are removed in
one operation. For example, removing both ovaries
and fallopian tubes is a bilateral salpingo-oophorectomy.
The other important surgical procedure
is debulking. In this procedure, the surgeon removes
as much tumor as possible, even though all of it can't
be removed. Most doctors believe this greatly improves
a patient's prognosis (outlook for survival). This
partial list of names of operations should help you
in understanding information you may read about ovarian
cancer and in discussing your cancer with your health
care professionals. Don't be afraid to ask your cancer
care team to explain your condition and recommend
treatments in simple, nonmedical terms.
It is important that your surgeon
is experienced in ovarian cancer surgery. Many general
gynecologists are not prepared to do the appropriate
cancer operation, which requires careful staging and,
perhaps, debulking. Ask your doctor if he or she is
experienced in treating ovarian cancer, can stage
your cancer properly, and can perform a debulking
procedure if that is needed. Otherwise you may need
a second operation.
Removal of both ovaries and/or the
uterus means that you will not be able to become pregnant.
It also means that you will go into menopause if you
have not done so already. Most women remain in the
hospital for 3 to 7 days after the operation and can
resume their usual activities within 4 to 6 weeks.
Surgery does not change your ability
to feel sexual pleasure. You do not need your uterus
to reach orgasm. Some women feel less feminine after
a hysterectomy; however, such thoughts do not reflect
the generally positive outcome concerning sexual function
and orgasm.
Chemotherapy
Systemic chemotherapy uses cancer
drugs that are injected into a vein or given by mouth.
These drugs enter the bloodstream and reach all areas
of the body, making this treatment potentially useful
for cancers that have metastasized (spread) beyond
the organ they started in.
Radiation Therapy
Radiation therapy uses high-energy
x-rays to kill cancer cells. These x-rays may be given
in a procedure that is much like having a diagnostic
x-ray.
External beam radiation therapy
In this procedure, radiation from
a machine outside the body is focused on the cancer.
External beam radiation therapy is one type of radiation
therapy used for treating ovarian cancer. Treatments
are given 5 days a week for several weeks. Each treatment
lasts only a few minutes and is similar to having
a diagnostic x-ray test. As with a diagnostic x-ray,
the radiation passes through the skin and other tissues
before it reaches the tumor. The actual radiation
exposure is very short, and most of the time is spent
precisely positioning the patient so that the radiation
is aimed accurately at the cancer.
Brachytherapy
Radiation therapy also may be given
as an implant of radioactive materials, called brachytherapy,
placed near the tumor or as a radioactive fluid placed
into the abdominal cavity. This is rarely done for
ovarian cancer.
|