|
Liver Tumor
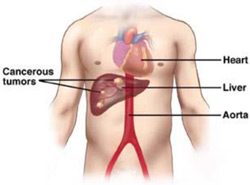 Malignant, or cancerous, liver tumors fall into two types: primary or metastatic. Primary tumors originate in the liver itself. Hepatocellular carcinoma is the most common type of primary liver cancer. Malignant, or cancerous, liver tumors fall into two types: primary or metastatic. Primary tumors originate in the liver itself. Hepatocellular carcinoma is the most common type of primary liver cancer.
Metastatic, or secondary, liver tumors have spread to the liver from a cancer elsewhere in the body. Because one of the liver's main functions is to filter blood, cancer cells from other parts of the body may become lodged in the liver and become tumors. The most common type of metastatic liver tumors are those caused by colon cancer that has spread to the liver.
Primary liver cancer, or hepatocellular carcinoma, is the most common type of cancer originating in the liver itself. (Most tumors in the liver do not originate there; they start elsewhere in the body and spread, or metastasize, to the liver.) In the United States, primary liver cancer is relatively rare -- it accounts for less than one percent of all cancers. But worldwide, hepatocellular carcinoma is the most common solid organ tumor. This is believed to be due to widespread viral hepatitis infection, a known risk factor for primary liver cancer.
Most primary liver cancers originate in the liver's parenchymal cells -- the cells that perform most of the organ's blood-filtering functions. Other rarer forms of primary liver cancer include peripheral cholangiocarcinoma (tumors in the sections of the bile ducts that are within the liver), sarcomas and angiosarcomas (cancer in the connective tissue of the liver), hemangioendotheliomas (tumors that arise in the blood vessels of the liver), and hepatoblastomas (a highly curable form of liver cancer most often found in children).
Hepatocellular carcinoma most commonly occurs in people whose livers have been damaged. This damage may be caused by alcohol abuse, by chronic infection with the hepatitis B or hepatitis C virus, from food contaminants called aflatoxins (though this is rare in the United States), or from metabolic diseases. Cancer can spread from the liver to other areas in the body through the blood or the lymph system, most often to the lungs, bones, and abdomen.
Several benign, or non-cancerous, tumors can occur in the liver. The most common form of benign tumor is called a hemangioma. Hemangiomas can occur anywhere in the body but occur most frequently in the skin and subcutaneous tissues (tissues beneath the skin). In nearly all cases, hemangiomas of the liver are harmless. In only rare instances do they cause pain or other problems. Once checked and deemed harmless, they can be left alone.
Hepatocellular cancer is one of the most common cancers in the world. As hepatitis B virus and hepatitis C are known risk factors for liver cancer, areas with higher rates of these infectious diseases -- including some areas of Africa, China, and Southeast Asia -- have higher rates of liver cancer. These viral infections are less prevalent in the United States, although the incidence of hepatitis C infection is growing.
Viral hepatitis is often a silent disease. The hepatitis virus can be present in the body for years and cause no pain or symptoms. As many as four million Americans may carry the hepatitis C virus, and most may not be aware that they are infected. Viral hepatitis is contracted through contact with infected blood or body fluids. In many cases, people became infected through blood transfusions administered before 1992 (before blood was first routinely screened for the disease). A small number of cases are still associated with recent blood transfusions. Intravenous drug users may become infected through contact with unsterilized needles. These infections are considered so serious that the U.S. Centers for Disease Control and Prevention issued guidelines in October 1998 requiring hospitals to track down and notify anyone who may have received infected blood prior to 1992.
Early in the infection hepatitis B can be treated with a combination of the anti-viral drugs alpha-interferon and ribavirin. In some cases the virus can be eradicated from the bloodstream and eliminated from the body. For this reason, doctors recommend that people at a high risk for developing the disease be screened. If the infection progresses, it can lead to chronic liver disease, or cirrhosis, a progressive disease of the liver, and, eventually, liver cancer. There is also a vaccine for hepatitis B. Doctors recommend that children, and those at high risk for developing the disease be vaccinated.
The risk of primary liver cancer is greater for those whose livers have been damaged by excessive alcohol consumption. Approximately 15 percent of alcoholics will develop cirrhosis of the liver. Cirrhosis also makes the surgical treatment of primary liver cancer more difficult.
Many patients with primary liver cancer have no symptoms. In some instances, jaundice, malaise, or a general feeling of poor health, loss of appetite, weight loss, fever, fatigue, bloating, itching, swelling of the legs, or weakness may be present. Abdominal pain or discomfort may also occur.
Diagnosis of primary liver cancer is generally made using blood tests, diagnostic imaging, surgical biopsy or laparoscopy, or a combination of the above. The alpha-fetoprotein blood test and ultrasound imaging of the liver are also used to screen high-risk populations (including those with hepatitis B and hepatitis C infections) for the disease. Since the risk of liver cancer is relatively low for healthy individuals, these tests are not used to screen the general population.
The alpha-fetoprotein (AFP) blood test measures the level in the blood of a certain protein produced by the liver. Elevated levels of AFP can be an indication of hepatocellular carcinoma, the most common type of primary liver cancer. If liver cancer is suspected, other blood tests are done to measure liver function. These tests can help doctors determine the condition of the liver. Since successful treatment for liver cancer involves removing a substantial part of the normal liver tissue in addition to the cancer, other treatments might be used in people with blood tests that indicate a high degree of liver disease.
As non-invasive diagnostic imaging techniques have become more sophisticated, they can be used to gather important information about a newly diagnosed tumor -- including its exact size, and density. These techniques can also be used to gauge how well a tumor will respond to treatment.
In some cases, diagnosis is performed invasively, by removing a small amount of tissue for a biopsy, or by laparoscopy (insertion of a small tube with an attached camera into the abdomen to survey the cancer site). Laparoscopy can also be used to remove a sample of tissue for biopsy.
Noninvasive Diagnostic Imaging Techniques
CT (computed tomography) scanning is useful for determining the extent of tumor growth within the gallbladder or bile duct. It can also be used to tell whether tumor cells have spread into the lymph nodes or other nearby parts of the body.
MRI (magnetic resonance imaging) can be used to determine if a tumor can be surgically removed. It shows the extent of tumor growth within the gallbladder or bile duct and reveals whether the tumor has invaded any blood vessels
Magnetic resonance cholangiopancreotography (MRCP) gives a detailed examination of the bile ducts. It is useful for determining the stage of a tumor in the bile duct.
Ultrasound useful for detecting the location and number of tumors as well as tumor involvement with blood vessels (tumors situated close to blood vessels may be more difficult to remove). It can also be used to distinguish a cancerous mass from a benign tumor.
Invasive Diagnostic Techniques
Biopsy a small amount of tissue is removed from a specific area of the body so it can be examined more closely.
Endoscopy the interior lining of a body cavity, such as the esophagus, stomach, bile duct, or colon, is examined using a device called an endoscope
Laparoscopy allows for the examination of the abdominal cavity and its contents. A tube with an attached camera (called a laparascope) is passed through an incision made in the abdominal wall.
Cholangiography a needle is inserted into the bile ducts within the liver. The ducts are injected with dye so they can be seen more clearly.
Treatment
For treatment purposes, primary liver tumors are classified in four ways. Localized and resectable tumors are found in one place and can be removed. Localized and unresectable tumors are found in one area but cannot be totally removed safely. In advanced cases, cancer has spread throughout the liver and/or to other parts of the body. In recurrent cases, the cancer has returned to the liver or another part of the body after initial treatment.
Surgery
Most primary liver cancers are best treated by surgery to remove the diseased portion of the liver. Until the early 1980s, surgery to remove primary liver tumors was rarely done. But now highly complex liver operations are performed with great frequency, success, and safety at AHMT Memorial Centre. Our researchers have recently shown that hepatobiliary surgery can also be successfully performed in elderly patients. These patients can have outcomes comparable to those of younger patients, so chronological age alone should not be the determining factor when deciding upon surgery in patients over the age of 70.
Operating on the liver can be difficult for several reasons. Many of the major blood vessels to and from the heart pass behind or through the liver, so in essence, the liver is "attached" to the heart. Also, the anatomy of the liver is not always obvious from the surface. The organ is large, dense, and delicate, and covered in part by the rib cage. It bleeds profusely when injured and it tears easily. Since hepatocellular cancer is relatively rare in the United States, many surgeons may not be experienced in performing liver resections. Our surgeons perform the highest number of liver resections of any cancer center in the country -- 200 to 300 per year.
The liver has the capacity to regenerate: Up to 80 percent of the organ can be surgically removed and within several weeks, the liver will have entirely regenerated itself. If one lobe--along with its associated blood vessels--is surgically removed, the remaining lobe will compensate for the loss. A new technique which stimulates regeneration before surgery is also being evaluated here. The technique is called pre-operative portal vein embolization. If doctors feel the portion of the liver remaining after resection would be too small to allow for a good outcome, they can shift the blood supply to the normal portion of the liver before the resection is done. That normal area grows larger, and when it reaches sufficient size, the resection can be performed.
When the liver is burdened with another disease aside from the cancer, surgery is complicated and sometimes impossible. A disease such as cirrhosis dramatically weakens the liver and often leaves it permanently damaged, with limited regenerative capacity. A patient with a liver hampered by both cirrhosis and a tumor is more likely to be treated with a method other than surgery. Some of these treatments are listed below.
Ablative Therapies
Ablation uses a chemical agent or energy to destroy a tumor. Ablative procedures can be performed both percutaneously (through the skin without an incision) or during surgery. Procedures which can be performed percutaneously include cryosurgery (freezing and killing the tumor cells), radiofrequency (RF) ablation, alcohol ablation, and embolization. These therapies can be very effective but are usually intended to control cancer rather than cure it.
Ablative therapies can be used alone or in combination with surgical removal of a tumor. For example, a patient with hepatocellular cancer who is not a candidate for surgery may first be treated with embolization to shrink the tumor so that it is small enough to make another form of ablative therapy or surgery possible.
In cryosurgery, a needle is introduced into the middle of a tumor to freeze it. Residual tumor cells can be left behind, making this method less effective than surgery. It can also be difficult to keep the tumor at temperatures low enough to completely freeze it, since tumors are often near large blood vessels. Nevertheless, cryosurgery can be a very effective way to control liver tumors.
Radiofrequency ablation is the opposite of cryosurgery. Rather than freezing the tumor, physicians use radio waves to heat it up to such a high temperature that the tumor is destroyed. RF ablation is effective, but can only be used for smaller tumors. This therapy is not curative; it is intended to control tumor growth.
Alcohol ablation or PEIT (percutaneous ethanol injection treatment) is a means of administering toxins directly to a tumor. It is quite effective for small tumors of less than 5 cm. This treatment is usually selected for patients who are not candidates for surgery.
Radiation Therapy
Radiation therapy is used in selected cases to help control tumors. Radiation oncologists here use new techniques to focus the radiation beam on the tumor and spare the normal liver from injury.
Embolization
Embolization is a procedure that cuts off the blood supply to the tumor. Physicians pack a branch of the hepatic artery -- the main artery that carries blood to the liver -- with tiny plastic particles, cutting off most of the blood flow and depriving the tumor of life-giving oxygen.
Amazon will work with you and our India
Affiliates to create a package where all your Cancer
concerns/problems can be addressed. If you have any
questions, please do not hesitate to contact us by
phone or email.
|