|
Bladder cancers
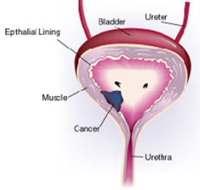 Of the three main types of bladder cancers, the most common is transitional cell carcinoma. Less common bladder cancers include squamous cell carcinomas and adenocarcinomas. Of the three main types of bladder cancers, the most common is transitional cell carcinoma. Less common bladder cancers include squamous cell carcinomas and adenocarcinomas.
A patientís treatment and survival rate depend on how deeply the cancer has invaded the bladder, and if it has spread to surrounding or distant sites.
The most common symptom of bladder cancer is blood in the urine. This symptom is usually painless, and is not always visible to the naked eye. Often, the diagnosis of bladder cancer is delayed because bleeding is intermittent. Other symptoms include an increased frequency of urination, an increased urgency to urinate, feeling the need to urinate but not being able to, and painful urination.
If you have one or more of these symptoms, it does not mean that you have bladder cancer. However, it is important to see a doctor so that any illness can be diagnosed and treated as early as possible.
Bladder cancer is most often diagnosed by examining cells in the urine under a microscope and by inspecting the bladder with a cystoscope -- a slender tube fitted with a lens and a light that is inserted into the bladder through the urethra.
If cancer is suspected, a tissue sample is removed during the cystoscopic procedure and examined under a microscope. If cancer is confirmed, computed topography (CT) may also be needed to determine the stage of the cancer -- whether the cancer is confined to the bladder or whether it has spread to other parts of the body, such as the lymph nodes, lungs, bones, or liver. Research is under way at AHMT Memorial Centre to determine if magnetic resonance imaging (MRI) and positron emission tomography (PET) can more accurately diagnose and stage bladder cancer.
Treatment
Treatment for bladder cancer varies greatly depending on the stage of disease at the time of diagnosis.
Superficial Bladder Cancer
The majority of bladder cancers are transitional cell carcinomas (TCC) that are confined to the lining of the bladder. The standard treatment for superficial bladder cancer is minimally invasive surgery using a cystoscope to remove the tumor.
Invasive Bladder Cancer
Surgery to remove the bladder is the most common treatment for invasive bladder cancer -- cancer that has spread into or beyond the muscle layer of the bladder wall -- and provides the best opportunity for a long-term cure for most patients.
For patients whose tumors require surgery to remove the entire bladder, it is also necessary to remove the surrounding lymph nodes to help prevent cancer recurrence or metastasis. In women, this procedure also involves the removal of the lower portion of the ureters, the uterus, fallopian tubes, the ovaries, and sometimes part of the vaginal wall and the urethra. In men, the prostate gland, the lower portion of the ureters, and sometimes the urethra are removed. After removing the bladder, surgeons must create a new way for the body to store and eliminate urine. The historical approach, called an ileal conduit, required a patient to wear a bag on the outside of the body to collect urine. During this procedure, a conduit for the urine was created using a segment of the small intestine. It transferred urine directly from the kidneys and ureters, and required a stoma on the skin to funnel the urine into the collection bag.
For people whose urethra has been removed, an internal bladder is created and then attached directly to the abdominal wall. A stoma is attached to the internal bladder, and the patient inserts a catheter into the stoma to eliminate the stored urine. It takes about three to five minutes to empty the bladder this way.
Many patients with muscle-invasive bladder cancer are treated with chemotherapy before or after surgery, using M-VAC or other regimens that have fewer side effects, to help prevent the recurrence of cancer.
Amazon will work with you and our India
Affiliates to create a package where all your Cancer
concerns/problems can be addressed. If you have any
questions, please do not hesitate to contact us by
phone or email.
|