| Radiofrequency
Ablation
Description
RFA of liver, lung and bone tumors
Preparation/Instructions
Pre-procedure workup
This is a method for treating some
tumors using the concept of thermal ablation. We currently
offer RFA of osteoid osteomas, other painful bone
metastases, lung cancers and liver cancers.
What is RFA?
RFA is a technique
that uses thermal ablation to "cook" lesions.
Using an electrode and an RF generation adequate heat
is generated inside a tumor, by placing the electrode
within the tumor.

RFA is a well-validated
technique for the treatment of liver and lung cancers,
for the ablation of osteoid osteomas and for treating
the pain associated with bone metastases. It has also
been used for adrenal tumors as well as sporadically
in other sites.
Procedure
- We first assess the tumor in detail, using CT
scans and MRI, which are performed at our centre.
However, if these investigations have already been
done, we go through them carefully.
- If the lesion is suitable for an RFA procedure
from the treatment perspective, we assess the technical
feasibility.
- If the lesion is technically accessible, then
a pre-procedure work-up is performed, which consists
of a basic health assessment, and the coagulation
profile.
- If there is no contraindication, the procedure
is then performed under deep sedation, with an anesthetist
in attendance.
- The procedure for an osteoid osteoma takes upto
30-45 minutes. For all other tumors, it may take
from 30mins to 2 hours depending on the size of
the tumor.
- After the procedure, the patient is observed
in the post-procedure room, until he/she is fully
conscious. Usually within three hours, the patient
leaves our centre. The patient is allowed light
food four hours after the procedure. The patient
will be on oral antibiotic coverage for another
3 days.
- With most tumors including osteoid osteomas,
the patient can go back to sedentary, non-strenuous
work within 24-48 hours.
Osteoid Osteoma
Points
- Osteoid osteoma is a common benign bone tumor
that occurs typically in the long bones
- Traditional treatment involves surgery and en-bloc
resection
- Radiofrequency thermal ablation (RFA) can "cure"
the lesion on an out-patient basis, using just deep
sedation
An osteoid osteoma is a benign
bone neoplasm that occurs typically in the long bones,
such as the tibia or the fibula in about 50% of cases,
in the diaphyseal or meta-diaphyseal cortex (Fig.
1). It is a relatively common neoplasm, representing
about 12% of all primary bone neoplasms.
The typical age group is between
5 and 25 years of age (>75%) and more common in
men. Patients with osteoid osteomas typically have
pain, which become worse at night and which responds
to anti-inflammatory drugs.
Radiologically, an osteoid osteoma
has a typical appearance of cortical thickening and
sclerosis. A nidus may not always be seen on plain
radiographs, but will always be identified on CT (Fig.
1). On MRI, there is marrow edema with peri-osseous
edema and usually the nidus is well visualized (Fig.
2).
Fig. 1:
(A, B): Osteoid osteoma. Plain radiograph (A) and
CT (B) showing a typical meta-diaphyseal, cortical
osteoid osteoma involving the upper end of the femur.
The nidus is well seen (red arrow) with the surrounding
cortical thickening (blue arrow).
Fig. 2:
Osteoid osteoma. MRI shows the nidus (red arrow) along
with marrow edema (blue arrow).
Traditionally, an osteoid osteoma
has been treated with en-bloc resection and surgery.
Though the results are good (85-95%), the complication
rates are high, including fracture at the site of
excision.
Among other alternative techniques
is radiofrequency ablation (RFA). The principle of
RFA is to induce thermal coagulation in the lesion
and to "cook" the lesion to death. Cure
rates with RFA are between 80-90%, with a 100% cure
rate for a second sitting, if the lesion recurs. The
complication rate is less than 2%.
The procedure is performed on an
outpatient basis. After the lesion has been localized,
deep sedation is given. A bone-biopsy trephine needle
is inserted into the nidus. Through this needle, the
RFA electrode is introduced (Figs. 3, 4). A temperature
of approx. 100 degrees Celsius is applied for 3 minutes.
If necessary, this cycle is repeated once more
Technical success is defined as
the ability to put the RFA electrode into the nidus.
Clinical success is defined as absence of pain after
24 hours following the procedure.
The patient is discharged the moment
the effect of the anesthesia has worn-off and the
patient has regained consciousness. A post-procedural
course of antibiotics and anti-inflammatory drugs
is prescribed.
On CT, there are no immediate signs
of cure. In about 50% of patients, the lesion undergoes
complete sclerosis at the end of six months, partial
sclerosis in another 25% and no change in 25%. Therefore
procedure success is purely measured on clinical grounds;
i.e. disappearance of the typical pain associated
with the lesion. On MRI, marrow edema
is often seen around the site of ablation, demarcating
the area of coagulation necrosis (Fig. 4C).

Fig:3
Osteoid osteoma of the femur. CT shows the position
of the electrode within the nidus (red arrow).
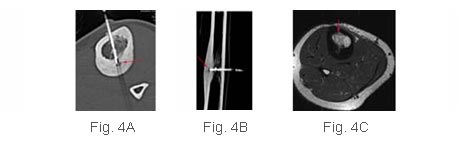
Fig.
4 (A, B, C): Osteoid osteoma of the tibia.
CT shows the position of the electrode (red arrow)
within the nidus, in the axial (A) and longitudinal
(B) planes. The post-procedure MRI shows the area
of coagulation necrosis (red arrow) surrounding the
nidus.
Complications |
Contraindications |
| 1. Thermal burns due to improper
grounding or selectrode placement |
1. Lesions within 1cm of a
major neurovascular bundle |
| 2. Procedural pain and discomfort |
2. Inability to withstand deep
sedation |
Cancers (lung, liver,
kidney, painful bone metastases)
RFA is an excellent method of treatment
for liver, lung and renal tumors.
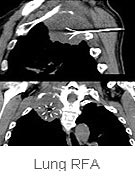 In
the lung, RFA is indicated in all situations where
surgery would be indicated, but is not being performed
due to either other co-morbid conditions that would
make surgery risky or when the patient refuses. It
is also performed when surgery is not the method of
choice, to supplement radiotherapy or chemotherapy
for associated metastatic disease. In
the lung, RFA is indicated in all situations where
surgery would be indicated, but is not being performed
due to either other co-morbid conditions that would
make surgery risky or when the patient refuses. It
is also performed when surgery is not the method of
choice, to supplement radiotherapy or chemotherapy
for associated metastatic disease.
 For painful bone metastases, RFA helps in alleviating
the pain. If the lesion is ablated in its entiretly,
it may not recur. If it does, re-ablation can be performed
as well. For painful bone metastases, RFA helps in alleviating
the pain. If the lesion is ablated in its entiretly,
it may not recur. If it does, re-ablation can be performed
as well.
In the liver, RFA is used in the treatment of hepatomas
and metastatic disease and the results have been consistently
good.
In the kidneys, RFA is again used
for small tumors, where surgery is contraindicated,
usually due to co-morbid conditions and survival is
almost similar to surgery.
|